Home » The Complete Guide to DBT
The Complete Guide to Dialectical Behavioural Therapy
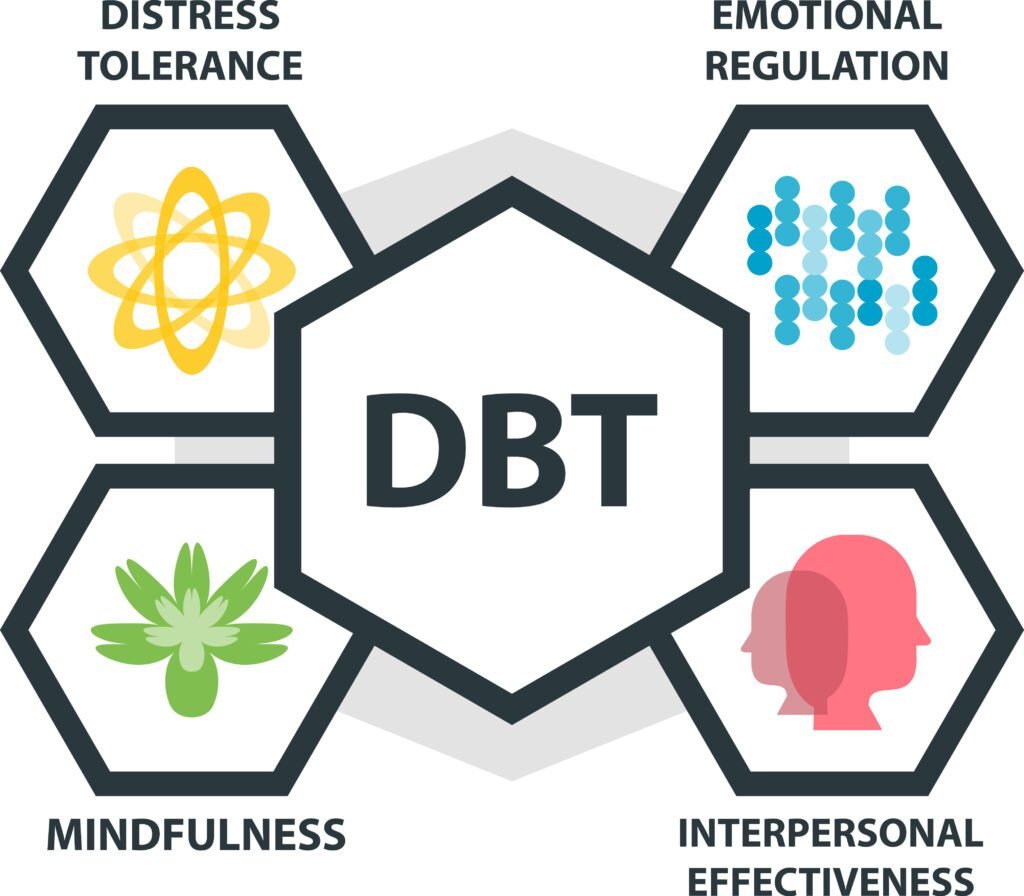
Understand how dialectical behavioural therapy can effectively teach patients techniques such as mindfulness and emotional regulation, providing valuable tools for managing personal challenges and enhancing overall well-being.
What is Dialectical Behavioural Therapy?
Dialectical Behavioral Therapy (DBT) is a proven, evidence-based form of talk therapy designed to equip individuals with new skills and strategies to help them build lives they find meaningful and fulfilling. While it is often used to treat borderline personality disorder, DBT is also highly effective for addressing a range of other mental health conditions.
DBT was first introduced in the 1970s by American psychologist Marsha Linehan. It was originally developed for the treatment of suicidal behaviours and borderline personality disorder but has since expanded to treat other complex mental health disorders.
DBT is rooted in Cognitive Behavioral Therapy (CBT) but is specifically tailored for individuals who experience emotions with heightened intensity. CBT helps patients recognize how their thoughts influence their emotions and behaviors, with a focus on shifting negative patterns into more positive ones.
“Dialectical” refers to the concept of balancing opposites. In DBT, patients are taught two seemingly opposing strategies that complement each other effectively:
- Acceptance: their behaviours and experiences are valid
- Change: they must make positive changes to manage their emotions and better their lives
What is the goal of DBT?
The primary aim of DBT is to guide patients in acknowledging and accepting their unhelpful or negative thoughts, feelings, and behaviors, while equipping them with the tools and techniques to effectively transform these patterns.
The Six Techniques of DBT
1. Core Mindfulness
Mindfulness serves as the cornerstone for developing and applying other skills. It encourages patients to stay present and cultivate a non-judgmental awareness of their thoughts, feelings, and sensations without becoming overwhelmed. By practicing mindfulness, patients can slow down, remain calm, and effectively utilize healthy coping strategies.
2. Distress Tolerance
Distress tolerance techniques equip patients to handle intense emotions by teaching them self-acceptance and how to embrace their current circumstances. These methods highlight the significance of cultivating healthy habits and adopting more effective coping strategies.
Distress tolerance skills include:
Distraction techniques: These methods assist patients in enduring challenging situations that cannot be altered and are intended for use only when the problem cannot be resolved.
Acceptance strategies: Patients are taught to manage pain in healthier ways, focusing on processing rather than avoiding it, which helps prevent additional suffering.
TIPP techniques: TIPP, which stands for temperature, intense exercise, paced breathing, and progressive muscle relaxation, represents DBT’s essential crisis management skills, designed to quickly alleviate distress.
3. Interpersonal Effectiveness
Interpersonal effectiveness empowers patients to assert themselves confidently in their interactions with others while preserving positive relationships. They learn to express their needs, listen attentively, communicate more effectively, and uphold respect for both themselves and others.
This approach focuses on managing challenging emotions, minimizing conflict, and fostering healthier, more fulfilling relationships overall.
4. Emotion Regulation
Emotion regulation assists patients in managing and transforming intense emotions that can create difficulties in their daily lives. This approach emphasizes understanding, controlling, and modifying emotional responses, offering valuable tools for those who struggle with regulating their emotional responses.
5. Validation
This technique acknowledges and affirms an individual’s emotions and experiences, emphasizing the importance of validation in creating a supportive and secure environment. Validation helps patients feel understood throughout their therapy journey. Building a trusted relationship between the patient and therapist is a cornerstone of DBT and is essential for effective treatment.
6. Dialectical Thinking
Dialectical thinking encourages patients to no longer think in black and white; instead, it embraces the idea that seemingly opposite perspectives can both be true. The balance between both perspectives allows patients to accept the reality of their thoughts and behaviours while making positive changes.
Assumptions of DBT
Each therapeutic approach is built upon foundational beliefs. These are presumed truths, hypotheses, or accepted facts that form the basis of the therapeutic process. Though often implicit rather than explicitly stated, they function as guiding principles and operational rules for treatment.
DBT is similar in this regard. It functions based on a specific set of assumptions, but unlike some therapies, DBT explicitly articulates these guiding principles.
Inherent capability and desire for Improvement: Patients and individuals are doing the best they can with their current knowledge and abilities. They inherently want to improve their lives and achieve happiness.
Responsibility for change: Despite not causing all their problems, individuals are responsible for solving them. This requires a commitment to change, increased effort, and motivation.
Acknowledgment of emotional distress: Recognizing that those struggling with intense emotions, such as suicidal tendencies, face unbearable emotional pain that drives self-destructive behaviors as temporary coping mechanisms.
Focus on learning and adaptation: Effective therapy involves patients learning new, adaptive behaviors in all relevant contexts. Therapy emphasizes continuous learning and adaptation without labeling patients as failures.
Non-Judgmental support and problem-Solving: Identifying and changing the causes of problematic behavior is more effective than judging and blaming. Providing unconditional support to patients is crucial for fostering positive change.
Therapist and patient support: Both therapists and patients need support. Therapists require support to maintain their effectiveness, while patients need to be provided with effective ways to deal with their problems and emotions to lead fulfilling lives.
Conditions That DBT Can Treat Effectively
Borderline Personality Disorder (BPD)
Highly effective for BPD, DBT focuses on emotional regulation, distress tolerance, and improving relationships, and addressing the core challenges of the disorder.
Obsessive Compulsive Disorder (OCD)
DBT effectively supports individuals with OCD by providing mindfulness and distress tolerance techniques, helping them manage and reduce obsessive thoughts and compulsive behaviors.
ADHD
DBT helps individuals with ADHD by enhancing mindfulness and self-awareness, leading to better focus and control over impulsive actions.
Anxiety
DBT addresses anxiety by blending cognitive interventions with skills for emotional regulation and mindfulness, fostering greater emotional balance.
Substance Abuse
DBT effectively treats substance abuse by teaching strategies to cope with emotional distress and reducing dependence on substances as a means of escape.
Eating Disorders
DBT aids those with eating disorders by promoting emotional regulation and stress management, leading to healthier eating habits and body image perceptions.
Anger Management
DBT offers practical tools for anger management by increasing mindfulness, helping individuals recognize and control their anger before it escalates.
Self Harm
For self-harm, DBT provides alternative coping mechanisms and emotional regulation techniques, reducing the urge to engage in self-destructive behaviors.
Suicidal Thoughts
DBT is effective in mitigating suicidal thoughts by enhancing problem-solving skills, emotional stability, and offering hope through improved distress tolerance.
The Main Benefits of DBT
1. Better Emotional Regulation
DBT empowers patients to understand, manage, and accept their emotions and behaviors. Through therapy, they learn to identify and become more aware of their emotions, enabling them to cope effectively with challenging situations.
2. Enhanced Interpersonal Effectiveness
DBT equips patients with the tools to set boundaries, become more assertive, and gain a clearer understanding of their needs while improving their ability to communicate effectively. This is valuable for everyone but particularly crucial for individuals with mental health conditions like social anxiety and ADHD. As a result, healthier and more fulfilling relationships are often formed through DBT.
3. Increased Mindfulness
Mindfulness is one of the core skills in DBT, guiding patients to be fully present in the moment. By practicing mindfulness, patients can more easily manage difficult emotions, enhance focus and concentration, and alleviate anxiety and stress.
4. Ability to Tolerate Distress
Distress tolerance equips patients with the ability to manage distressing emotions without turning to unhealthy coping mechanisms. Through this skill, patients build resilience and enhance their overall mental health. It is particularly beneficial for those dealing with impulsive behaviors and intense emotions.
5. Ability to Handle Crises
DBT teaches patients valuable skills to navigate crises effectively. They can rely on techniques like distraction, acceptance, and TIPP skills to support them during challenging times. These skills are especially beneficial for individuals dealing with trauma, anxiety disorders, and those who struggle to manage stress.
6. Improves Relationships
DBT promotes the development of healthy relationships and encourages patients to rely on their support network. Building a strong support system, grounded in trust and clear boundaries, is essential for managing mental health challenges and overcoming obstacles.
7. Improves Quality of Life
DBT not only enhances relationships but also significantly improves a patient’s overall quality of life. While mental health challenges may remain a part of someone’s life, DBT equips them with the tools to make positive changes. Upon completing therapy, patients can regulate their emotions and manage distress in a healthy and effective manner.
Considerations of Dialectical Behavioural Therapy
When considering Dialectical Behavioural Therapy, take these important factors into account:
DBT is not recommended for people with panic disorders:
DBT does not specifically address trauma processing, so individuals with panic disorders, such as PTSD, who need to heal from traumatic experiences might not find it fully beneficial on its own. Depending on their symptoms, patients may gain more from combining DBT with other therapeutic approaches.
DBT works best for motivated individuals who believe they need to change:
DBT is effective only for those who genuinely believe in the need for change. Patients must have a desire to develop new skills and be willing to recognize and address their unhealthy behaviors in order to make meaningful improvements.
DBT is structured and has strict boundaries that must be followed:
DBT demands a commitment to weekly therapy sessions, typically lasting six months to a year. Patients are required to engage in both one-on-one and group therapy sessions, as well as complete homework assignments to apply the skills they learn in real-life situations. With a wide range of skills and techniques involved, patients must be open to trying all of them to maximize their chances of success.
Schedule a Free Consultation
You don’t have to face your challenges alone. We specialize in dialectical behavioral therapy and are here to provide you with the support you need. Schedule a free consultation to start your journey and receive all the tools you need for a positive future and better well-being.